Endotracheal Intubation of an Adult
This assignment required the creation of a set of instructions for a complex topic. The assignment required use of smaller steps to achieve the overall task, use of clear language and visual aids/illustrations.
Introduction & Overview
These instructions will provide steps for endotracheal intubation of an adult, specifically orotracheal intubation. Nasotracheal intubation will not be covered by these instructions. The instructions are intended to be a resource for medical practitioners or students, to include but not be limited to physicians, registered nurses, paramedics and respiratory therapists. The scope of the instructions includes the intubation process of a patient who is already unconscious or who has already been provided rapid sequence induction or anesthesia. As such, the instructions will not cover the pharmacologic steps taken prior to an intubation, including the use of sedation or paralytics.
Equipment
Endotracheal tubes, 2 each, sizes 2.0 to 8.0
Laryngoscope handle with bulb and batteries
Laryngoscope blades
- Miller blades 0-4
- Macintosh blades 1-4
Bag-Valve-Mask (BVM), connected to oxygen source
Bougie device
Commercial endotracheal tube holder or tape
10cc syringe
Cardiac monitor, pulse oximetry and end tidal CO2 monitor
Stethoscope
Rescue airways (e.g. King Tube, CombiTube, Laryngeal Mask Airway (LMA), iGel)
Oropharyngeal airway kit
Process
Preparation
- Obtain pre-intubation history if available and time permits
- Prior intubation(s), dental problems, sensitivity or allergy to medications, cardiac or respiratory conditions, ear/nose/throat conditions
- Mallampati scoring
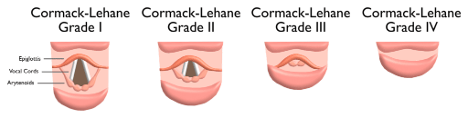 Figure 1
Figure 1
2. Prepare all necessary equipment and supplies, and ensure they are in operational order.
3. Position the patient supine on firm flat surface (e.g. gurney, operating room table, ground).
4. Preoxygenate the patient
- Provide 100% oxygen by ventilating the patient with a BVM connected to 100% oxygen
- Provider may use an oropharyngeal or nasopharyngeal airway as necessary to maintain a patent airway during preoxygenation.
 Figure 2
Figure 2
Perform laryngoscopy of patient
- Remove oropharyngeal or nasopharyngeal airway if used in above steps
- Insert laryngoscope blade into the right side of the patient’s mouth, sweeping the tongue to the left and up, while lifting the mandible (lower jaw) up and away from the patient
- Continue to advance the laryngoscope blade into the posterior oropharynx until the epiglottis can be visualized
- If using a Macintosh laryngoscope blade (fig. 5), insert the tip of the blade into the vallecula far enough to allow for enough pressure in the vallecula to lift the epiglottis
- If using a Miller laryngoscope blade (fig. 3,4), insert the tip of the blade enough to allow for lifting of the epiglottis, and lift the epiglottis with the tip of the blade

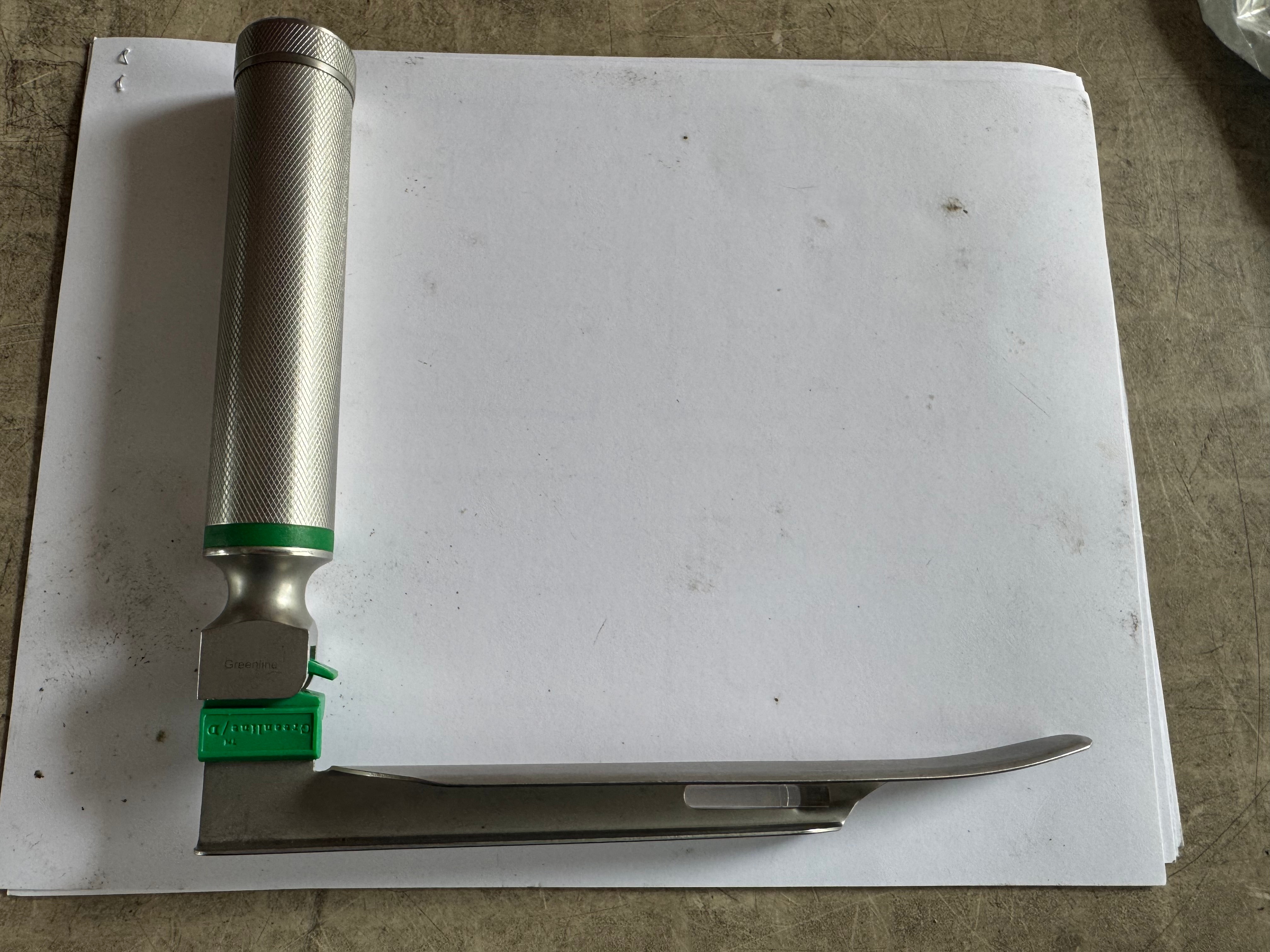
 Figures 3-5
Figures 3-5
4. Visualize the vocal cords. Once vocal cords are visualized, maintain view of the vocal cords until the patient is intubated or the intubation attempt is aborted-do not interrupt visualization.
- NOTE: A Cormack-Lehane score of grades 3 or 4 is considered a difficult airway.
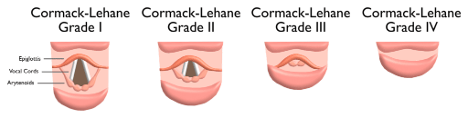 Figure 6
Figure 6
Intubate the patient
1. Suction the patient as necessary
2. Insert the appropriate size endotracheal tube into the right side of the patient’s mouth, maintaining a view of the vocal chords
3. Insert the endotracheal tube through the vocal chrds, visualizing the end of the tube passing through the vocal chords and continuing until the inflatable bladder is past the vocal chords approximately one centimeter. Notate the centimeter marking on the endotracheal tube that lines up with the patient’s teeth.
4. Remove the laryngoscope blade while maintaining the position of the endotracheal tube with one hand. Remove the stylete if used.
5. Inflate the bladder on the end of the endotracheal tube with 10cc of air via syringe attached to the inflation tube
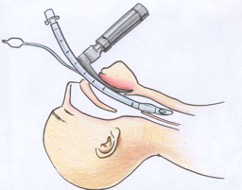
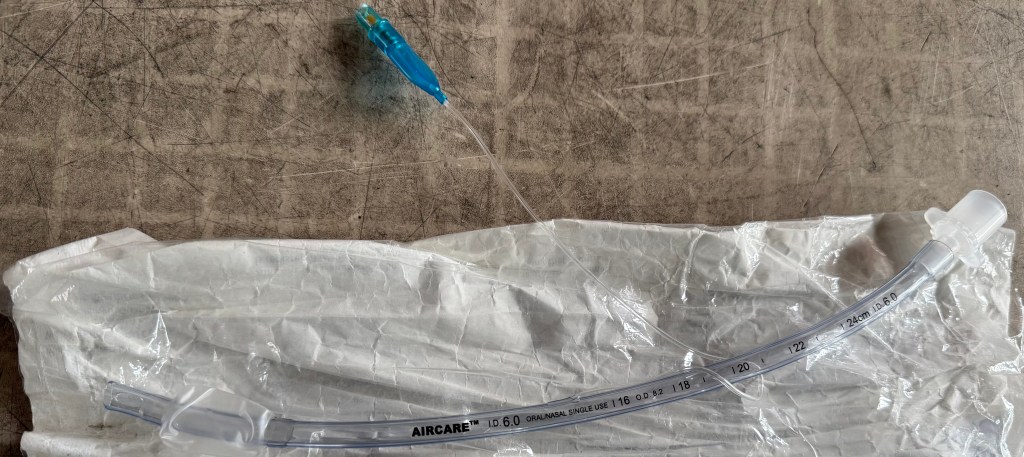
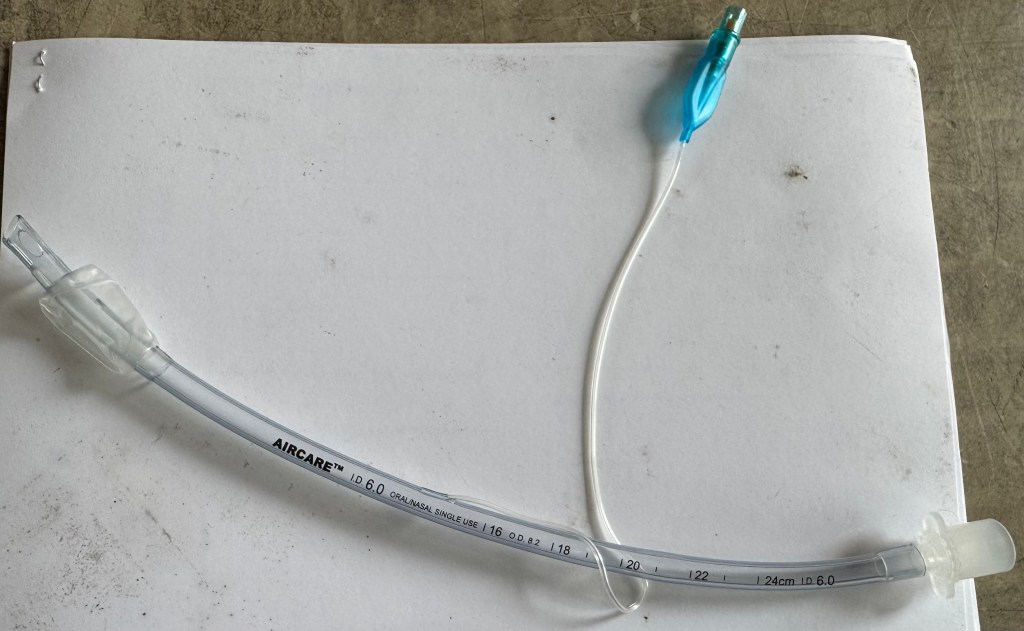
Figure 7a, b, c
Endotracheal Tube Placement Confirmation
- Confirm correct placement of the endotracheal tube by:
- Ventilating the patient through the endotracheal tube with a BVM connected to an oxygen source
- Auscultation over the epigastrium of the patient with a stethoscope and confirming the absence of breath sounds with BVM ventilations performed.
- Auscultation over the right and left sides of the chest, anteriorly and laterally, confirming the presence of breath sounds with BVM ventilations performed.
- Confirmation of End Tidal CO2 (ETCO2) presence
- Connect an inline ETCO2 detection device to the end of the tube, and the other end to a monitor with ETCO2 detection capability
- Confirm presence of ETCO2 through capnometry (numerical reading of ETCO2 level detected) and capnography (waveform illustrating ETCO2 level during each ventilation)
- If proper endotracheal tube placement cannot be confirmed with the above steps, remove the endotracheal tube and preoxygenate patient prior to reattempting intubation.
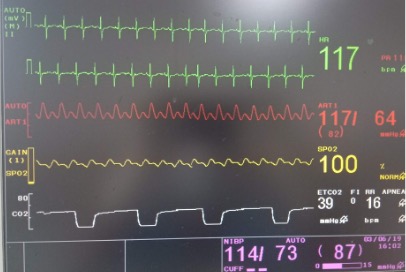
Figure 8
Secure the endotracheal tube
- Secure the endotracheal tube utilizing a commercial tube holder or tape
 Figure 9
Figure 9
Ventillation and Oxygenation
- Continue to ventilate patient with BVM (mask removed) connected to high flow oxygen, or attach a ventilator with inline oxygen supply
Difficult Airway/Emergency Procedures
Rescue Airways
- In the event of a difficult intubation, as determined by repeat unsuccessful intubation attempts, a poor Mallampati grade, and/or a Cormack-Lehane scale grade of 3 or 4, the following should be performed:
- Preoxygenate the patient between intubation attempts, or after a final attempt and prior to use of a rescue airway
- Secure an advanced rescue airway utilizing one of the following devices:
- CombiTube
- King LT-D Tube (Fig. 10c)
- Laryngeal Mask Airway (LMA) (Fig. 10b)
- iGel (Fig. 10a)


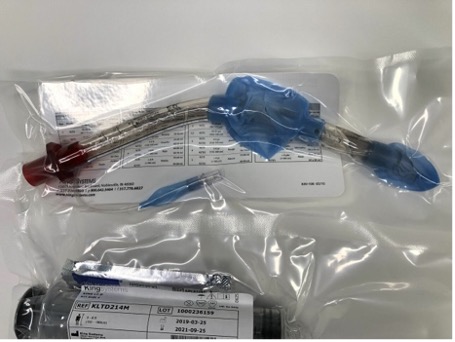
Figure 10a, b, c
Glossary
Bag-Valve-Mask (BVM): Also known as a manual resuscitator, and consisting of a bag, a valve and a mask, a BVM is a device which is utilized to provide artificial ventilations to a patient who is not breathing or breathing ineffectively.
Bougie: A long, thin plastic device inserted into the glottic opening and trachea during laryngoscopy, prior to inserting the endotracheal tube. Also called a tracheal tube introducer, once inserted, an endotracheal tube is passed over the bougie and inserted into the trachea through the glottic opening, and the bougie is then removed. Utilized in difficult intubations.
CombiTube: An esophageal-tracheal, double-lumen airway utilized as a rescue airway for difficult endotracheal intubations
Cormack-Lehane Score: A grading system which identifies the level of visibility of the epiglottis and glottic opening, and the ease or difficulty of the visualization, with a score of 1-4
Endotracheal tube: A plastic tube inserted into the trachea through the vocal chords to secure a patent airway in a patient unable to protect their own airway, or is otherwise in need of ventilatory support.
Epiglottis: A flap of cartilage located at the back of the tongue and above the glottic opening; covers the glottic opening while swallowing to prevent aspiration
iGel: A supraglottic airway utilized as a rescue airway for difficult endotracheal intubations
King LT-D Tube: Alternative/emergency advanced airway designed for blind placement into the esophagus, with the airway functioning as a supraglottic airway, utilized as a rescue airway for difficult endotracheal intubations
Laryngeal Mask Airway (LMA): A supraglottic airway consisting of a mask at the distal end of the tube which is placed over the supraglottic structures and the glottic opening; the LMA is utilized as an alternative to endotracheal intubation in some elective cases, or as a rescue airway for difficult endotracheal intubations
Laryngoscope: An instrument utilized to visualize the larynx, consisting of a handle containing batteries, and a blade which attaches to the handle equipped with a light bulb.
Laryngoscopy: A procedure where the larynx is visualized utilizing a laryngoscope
Macintosh blade: A curved laryngoscope blade available in sizes 1-4
Mallampati score: A test utilizing visualization of a patients open mouth to assess the relative size of the tongue base to the oropharynx, utilized to determine the level of difficulty of laryngoscopy and in establishing an advanced airway, i.e. endotracheal intubation
Miller blade: A straight laryngoscope blade available in sizes 00-4
Photo Credits
Figure 1: slidetodoc.com and multiple other websites
Figure 6: tactical-medicine.com
Figure 7a: vinmec.com
Figure 8: surgicaltechie.com
Figure 10b: healthproadvice.com
Figure 10c: ar.inspiredpencil.com
